Platelet Activation and Aggregation Promote Lung Inflammation and Influenza Virus Pathogenesis
Le VB, Schneider JG, Boergeling Y, Berri F, Ducatez M, Guerin JL, Adrian I, Errazuriz-Cerda E, Frasquilho S, Antunes L, Lina B, Bordet JC, Jandrot-Perrus M, Ludwig S, Riteau B
2014 • Am J Respir Crit Care Med • [pdf]
RATIONALE: The hallmark of severe influenza virus infection is excessive inflammation of the lungs. Platelets are activated during influenza, but their role in influenza virus pathogenesis and inflammatory responses is unknown.
OBJECTIVES: To determine the role of platelets during influenza A virus infections and propose new therapeutics against influenza.
METHODS: We used targeted gene deletion approaches and pharmacologic interventions to investigate the role of platelets during influenza virus infection in mice.
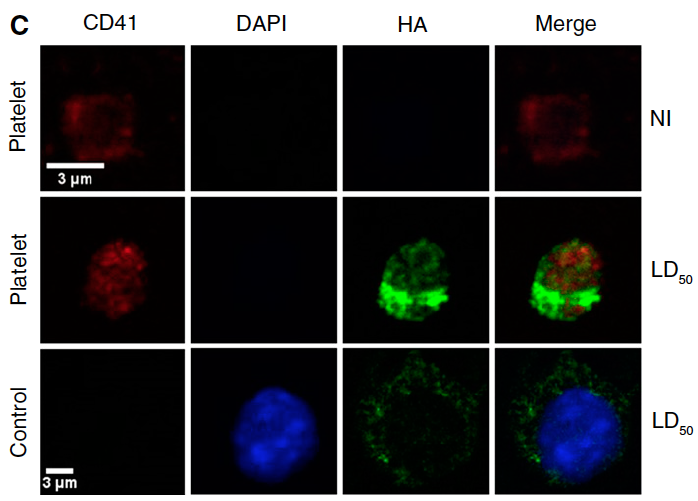
MEASUREMENTS AND MAIN RESULTS: Lungs of infected mice were massively infiltrated by aggregates of activated platelets. Platelet activation promoted influenza A virus pathogenesis. Activating protease-activated receptor 4, a platelet receptor for thrombin that is crucial for platelet activation, exacerbated influenza-induced acute lung injury and death. In contrast, deficiency in the major platelet receptor glycoprotein IIIa protected mice from death caused by influenza viruses, and treating the mice with a specific glycoprotein IIb/IIIa antagonist, eptifibatide, had the same effect. Interestingly, mice treated with other antiplatelet compounds (antagonists of protease-activated receptor 4, MRS 2179, and clopidogrel) were also protected from severe lung injury and lethal infections induced by several influenza strains.
CONCLUSIONS: The intricate relationship between hemostasis and inflammation has major consequences in influenza virus pathogenesis, and antiplatelet drugs might be explored to develop new antiinflammatory treatment against influenza virus infections.