Hemostatic disorders in a JAK2V617F-driven mouse model of myeloproliferative neoplasm
Lamrani L, Lacout C, Ollivier V, Denis CV, Gardiner E, Ho Tin Noe B, Vainchenker W, Villeval JL, Jandrot-Perrus M
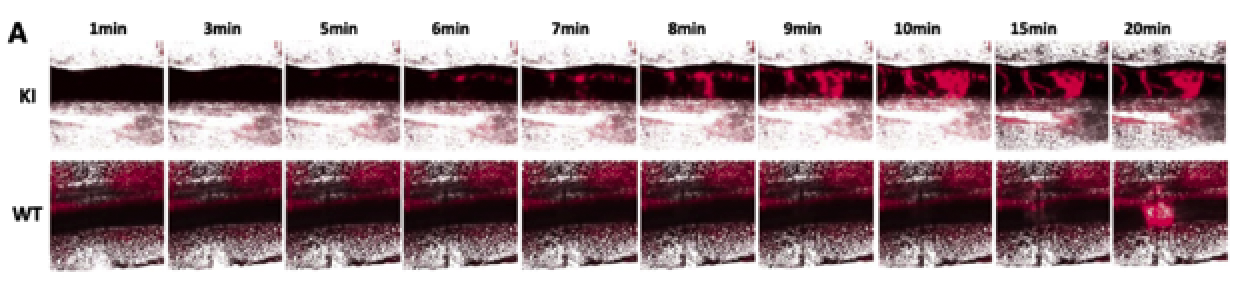
Thrombosis is common in patients suffering from myeloproliferative neoplasm (MPN), whereas bleeding is less frequent. JAK2(V617F), the main mutation involved in MPN, is considered as a risk factor for thrombosis, although the direct link between the mutation and hemostatic disorders is not strictly established. We investigated this question using conditional JAK2(V617F) knock-in mice with constitutive and inducible expression of JAK2(V617F) in hematopoietic cells, which develop a polycythemia vera (PV)-like disorder evolving into myelofibrosis. In vitro, thrombosis was markedly impaired with an 80% decrease in platelet-covered surface, when JAK2(V617F) blood was perfused at arterial shear over collagen. JAK2(V617F) platelets presented only a moderate glycoprotein (GP) VI deficiency not responsible for the defective platelet accumulation. In contrast, a decreased proportion of high-molecular-weight von Willebrand factor multimers could reduce platelet adhesion. Accordingly, the tail bleeding time was prolonged. In the FeCl3-induced thrombosis model, platelet aggregates formed rapidly but were highly unstable. Interestingly, vessels were considerably dilated. Thus, mice developing PV secondary to constitutive JAK2(V617F) expression exhibit a bleeding tendency combined with the accelerated formation of unstable clots, reminiscent of observations made in patients. Hemostatic defects were not concomitant with the induction of JAK2(V617F) expression, suggesting they were not directly caused by the mutation but were rather the consequence of perturbations in blood and vessel homeostasis.